Children’s mental health: barriers to a digital first approach
Using safe and engaging tech-powered interventions can equip anyone addressing the mental health needs of children and young people to achieve this in a timely and effective way.
To fully realise the positive impact of ‘digital first blended support models’, we must break out of the big box of all things tech and appreciate their diverse and unique capabilities.
The new normal
The world has been riding the tall and short waves of the pandemic for over a year. An entire generation of children are still adrift in the murky waters of disrupted school life, distant friendships and for many, loneliness and poor mental health.
There’s no surprise that a recent report from NHS Digital has found that youth referrals for mental health support have doubled since the pandemic started , and restricted access has meant that mental health services have been oversubscribed and staff members overstretched. All the while, hidden domestic traumas and hard to reach families have meant that the long term damage done is still hard to scope.
“The predicted levels of demand are two to three times that of current NHS mental health capacity within a 3-5 year window. This is not a scenario where services can grow incrementally to meet steadily rising levels of need. Instead, the Government and the NHS must take action now to meet a very steep increase in demand for mental health support.” (Centre for Mental Health)
Early intervention and prevention is an action item on everyone’s agenda along with tapping into the power of digital technologies - offering safe and remote access to support. In our everyday life, the role of technology has never been more significant in enabling the acceptance of safety measures as the new normal. Touch free payments, video conferencing and online services continue to evolve, improve and innovate - shifting our priorities, our behaviours and our relationship with technology.
Technology as an enabler
The new normal is demanding and impatient, putting services under immense pressure to fast track the provision of digital support where appropriate. More than ever, technology and the internet have become a lifeline for children and young people during lockdown and extended periods of social distancing. Laptops and mobile devices are a must have for every household in the UK. The Department of Education provided over 1.3 million laptops and tablets to support disadvantaged families with remote and face-to-face education during the COVID-19 pandemic.
Our healthcare system already has its work cut out to meet the expectations of a ‘digital first approach’ outlined in the NHS Long Term Plan:
“In ten years’ time, we expect the existing model of care to look markedly different. The NHS will offer a ‘digital first’ option for most, allowing for longer and richer face-to-face consultations with clinicians where patients want or need it.”
The reality is different as several barriers stand in the way of us realising this vision.
Barriers to a digital first approach
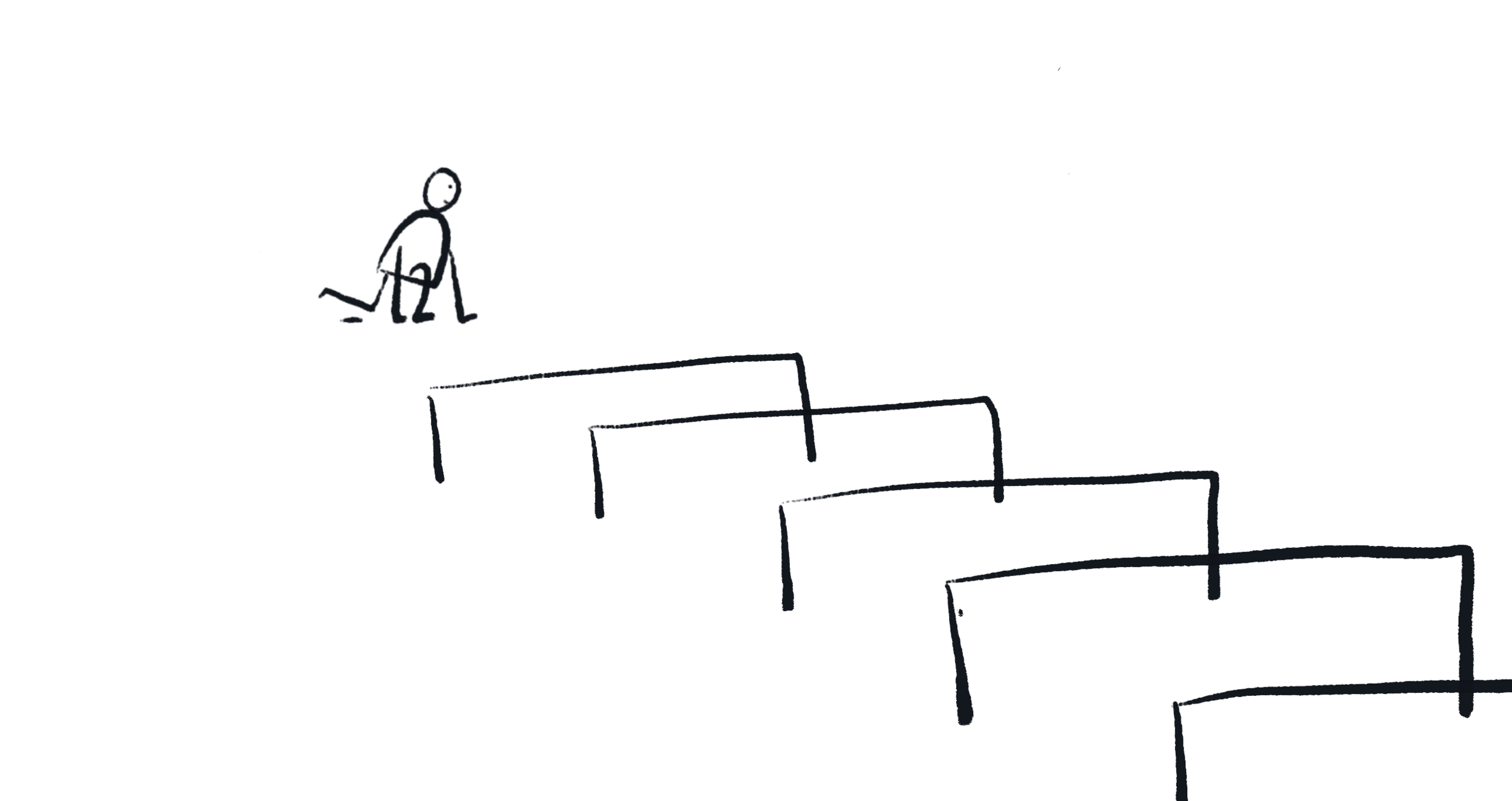
Services across the UK are lagging behind in fully realising the potential of digital technologies to aid the development of blended support models. Due to increased demand, national/regional targets and the NHS pushing for adoption of digital technologies - immense pressure has built up. Several decision makers end up checking the ‘digital checkbox’ by commissioning ‘a convenient solution’ rather than the most ‘effective one’ in terms of health outcomes, usability and cost. There are several reasons for this:
1. I’m just not that ‘techy’
Healthcare and technology are two areas that are very different in their respective natures. Furthermore, technology is evolving at a rapid pace as this report by Health Education England points out:
“The pace of technological change is a challenge to us all in maintaining and improving our digital capabilities in order to provide the best care.”
This rapid transition has left many healthcare professionals not feeling ‘techy’ enough. Less familiarity, low confidence and often unwillingness topped by the lack of policy and investment in digital literacy at an organisational level can contribute to professionals feeling unequipped. This presents a huge challenge for key decision makers responsible for providing digital support services to children and young people that is well informed and considered.
2. Bad experiences with inferior products
There are hundreds of digital apps for CYP making similar claims. To add to the confusion, tech powered solutions are extremely diverse in terms of their complexity and capabilities, e.g. an SMS service is very different from a wearable capturing patterns of heart rate variability. Yet, all things technological or digital are often lumped into one big box. Apps are simply a format in which innovators package their solutions - each with their intended impact. Comparing apps without understanding their full functionality often leads to an uninformed response such as:
“We tried something similar and it was terrible”.
The lack of understanding of the diverse capabilities of digital options, topped with multiple solutions making similar claims can be a real challenge. The NHS’s Digital Technology Assessment Criteria for health and social care (DTAC) is the most holistic and current assessment tool giving staff and patients confidence that the digital health tools they use meet their clinical safety, data protection, technical security, interoperability and usability and accessibility standards.
3. Fear of adopting new innovations
One reason for this can be our perception of ‘good’ and lack of understanding around tech powered solutions. The other may be the fear that tech powered solutions are designed to replace humans. In most instances, tech powered solutions are being used to further support, minimise inefficiencies and address unmet needs. Yet, we struggle to rise above our own insecurities and leverage the ways in which we can further support systems, improve access, meet unmet needs, empower professionals and provide better health outcomes.
4. Stack of evidence before use
A unique aspect about tech powered solutions designed for service users is that users present emergent behaviours as they start their journey with the tech solution. These behaviours are learnt, understood and then fed into further refinement of the tech solution. So, it really only becomes its most user friendly and effective version when put into the hands of users.
However, to minimise risks healthcare demands that full evidence, design and functionality be determined well before the technological solution reaches users. This can be a challenge not only when innovating but also when commissioning. Digital health tools must go through long and rigorous periods of evidence building prior to reaching real service users. RCTs and Trials can be expensive and time consuming and many new innovators in health tech will most likely run out of resources at this point.
5. Budget Holders are hard to reach
All solutions (irrespective of the industries they serve) go through an innovation process of validation, iteration and refinement. Opportunities for constructive feedback and early screening by budget holders in healthcare is vital for new health tech innovations. This can help ensure that new innovations are helping alleviate the right pain points in an effective way.
However, budget holders are incredibly hard to reach until the point where a solution may be fully baked, missing out on being able to inform the innovation’s development journey to better align with their service needs. As a result, a lot of solutions never achieve their aims and healthcare continues to struggle to meet demand.
While several new innovations are emerging along with the NHS, DfE and other organisations channeling their efforts towards faster adoption of effective digital technologies, the long hard journey will continue unless we overcome these barriers.
It is critical that we reach a point where healthcare and technology are well aligned to effectively influence and adopt appropriate support models with a digital first approach to ensure that generations of children and young people don’t carry the burden of life long ill mental health.
Next time...
How can digital technologies enrich blended models of support for better children and young people’s mental health? Stay tuned for my next article where I’ll share a visual framework and insights that can help you on your journey of realising truly blended models of support.